Digitized Surgical Care Pathways Speed Up the Patient Flow
Automation is increasingly finding its way into business processes and productivity tools. With its ability to automate many of the steps necessary to perform a specific task, automation is capable of optimizing tasks and improving efficiency. Because of this, automation is a significant part of different business strategies. One industry that's also benefiting from automation is the healthcare industry.
Automation in healthcare provides benefits such as:
- Cost of care savings
- Improved care quality and consistency
- Increased predictability of outcomes
- Data-driven insights
One very promising area is speeding up and optimizing the surgical care pathway of a patient. Not only does this mean that the patient gets treatment faster, but also that the patient's treatment is better, simply because the process is optimized for patient care and provider productivity.
But how can a digitized surgical care pathway speed up the patient flow? With this post, we’ll take a look at this question in more detail.
What Is Surgical Patient Flow?
So, what exactly is surgical patient flow?
In simple terms, patient flow is the movement of patients through a healthcare facility like a hospital or clinic. It involves every step of the patient from the point of admission to the point of discharge and involves the medical care, physical resources, and internal systems needed to get the patient through the flow while maintaining quality and patient satisfaction.
Logically, surgical patient flow is then the path a patient follows from admission for a surgery, through the surgery, the aftercare procedures in hospital, up to discharge after the surgery. It involves everything and every provider involved in the process.
Considering that optimized patient flow is important for quality and patient satisfaction, there are some hospital patient flow best practices that should be followed. These include:
- Creating processes that facilitate good patient flow throughout the hospital, including the surgery departments.
- Addressing what happens when beds aren't ready for admitted patients or patients are not qualified for their operation due to a patient did not follow fasting or medication instructions.
- Making sure that patients who are diverted to overflow areas receive proper care.
- Formalizing how ambulance diversion decisions are made and implemented.
- Setting patient flow goals and measuring progress towards those goals and taking improvement actions when the goals are not achieved.
- Managing patient “boarding” and working to reduce the length of time that it takes for emergency department patients to be boarded.
- Constantly reviewing results of flow management initiatives against the stated goals and taking action when those goals are not achieved.
- Working closely with behavioral health providers to provide better coordinated care.
Attention should be paid to distinguishing the surgical patient flow from a surgical care pathway.
In contrast to surgical patient flow that takes place in hospital, the surgical care pathway involves every step from when the patient is scheduled for surgery up to the stage where patient has completely recovered after the surgery. In other words, the surgical care pathway addresses every point in the surgery cycle.
For this reason, the surgical care pathway is typically broken up into five phases:
- The preoperative phase. These are the processes that are administered before a surgery in order to prepare a patient.
- The perioperative phase. These are the processes that are administered at or around the time of surgery.
- The intraoperative phase. These are the processes that occur or are performed during the course of a surgery.
- The postoperative phase. These are the processes that occur following a surgery.
- The post discharge phase. These are the processes that are administered once a patient is discharged from hospital following a surgery.
To ensure the most optimized process, surgical patient flow management is vital, and that’s where a digital surgical care pathways can help.
The Digital Surgical Care Pathway
In order to optimize the surgical care pathway, health care facilities can take advantage of a digital surgery patient management platforms like the BuddyCare platform. They help facilities create surgical care pathways for patients and automate large parts of the process including all patient communication and patient data collection.
There is clear communication and collaboration between doctors and patients during which patients are guided through each phase of the surgery, ensuring that they understand all the processes involved, know what to expect, and how they can prepare for it mentally, emotionally, and physically.
A typical automated surgical patient care pathway will look like this:
- The first step - The hospital invites the patient as a digital patient on the BuddyCare platform, which gives the patient an opportunity to access the app with an activation code. Keep in mind that, prior to this, the patient would have typically visited the hospital for a treatment assessment and would have been put on the surgical waiting list. Once a slot opens up, a time for the surgery would have been set.
- Second step - The patient will receive care-related education materials and instructions on an interactive timeline that guides the patient through the process. This step signals the first step of the preoperative phase.
- Third step - The patient will get the opportunity to fill in an anesthesia questionnaire.
- Fourth step - As the surgery approaches, automatic reminders will be sent to the patient that reminds them when to stop eating, drinking, and taking medications.
- Fifth step - On the day before the surgery, the patient will receive a pre-surgery checklist and a digital pre-assessment form that ensures the patient's eligible for surgery.
- Sixth step - Up to this stage, and on surgery day, it means that the patient is completely ready for surgery and that there are no outstanding issues.
- Seventh step - Once the surgery is completed and the patient enters the post-surgery phase, early mobilization after the surgery will be encouraged and supported through the app.
- Eighth step - The patient will receive educational materials and videos to stay on track with their recovery plan.
- Ninth step - The patient will be given the opportunity to complete post-operative surveys and scorecards during which the hospital can gather data to analyze and improve their processes and outcomes where necessary.
- Tenth step - Lastly, the patient will be encouraged to follow evidence-based best practices for enhanced recovery after the surgery (ERAS).
By following this surgical care pathway, the patient’s care and recovery is optimized without much intervention from the care team, because many of these steps are automated.
Benefits of a Digital Surgical Care Pathway
Now apart from the benefits listed above, digital surgical care pathways offer a variety of other benefits which all help with optimizing the process:
Better and Automated Patient Communication
Without a digital surgical care pathway, the main form of communication with patients is calling and sending letters or emails. This requires a lot of time and effort. An efficient surgery patient management or care coordination system can help hospitals improve operational efficiency by automating and optimizing timed patient communication.
For example, Buddy Healthcare’s patient-facing app educates and reminds patients about upcoming tasks or appointments automatically and the patient is always aware what's coming next, what steps need to be taken, and which tasks need to be completed.
It also has a helpful timeline feature that provides patients with all the information related to their care. With these features, patients then receive preoperative assessments and other forms and in-app questionnaires automatically in a digital format and thus can submit tasks and questionnaires at own pace 24/7.
They also receive care-related pre- and postoperative education and are given appointment and task reminders to keep them on track. This means that patients can receive information about the operation, procedure checklists, educational videos or photos, advice on when to start or stop taking medication, rehabilitation exercises, and more. Everything is completed automated and delivered through the app.
This does not only make sure that the patient is ready on the day of the surgery, but also goes a long way to ensure that patients are well informed and less anxious about their upcoming procedure. Combined, this means optimal patient care.
Better Patient Care
While patients use the mobile app to, for instance, log their pain on a pain scale, complete questionnaires, or send secure messages to care teams, the care personnel dashboard gives medical staff a real-time 360 degrees overview of all their patients pre- and postoperative preparation tasks.
Here, the care team can, for example, see whether the patients have read all the educational materials, submitted the preoperative assessments or other questionnaires, and followed dietary and medication instructions.
Likewise, in the postoperative phase, the care team can monitor whether patients have completed the post-operative exercises, view pain scale measures in real-time and collect electronic patient-reported outcomes and patient-reported experience measures.
Streamlined Care Process
The biggest advantage to the system is that it greatly increases operational efficiency due to several reasons.
For one, the surgical care pathway is shortened considerably.
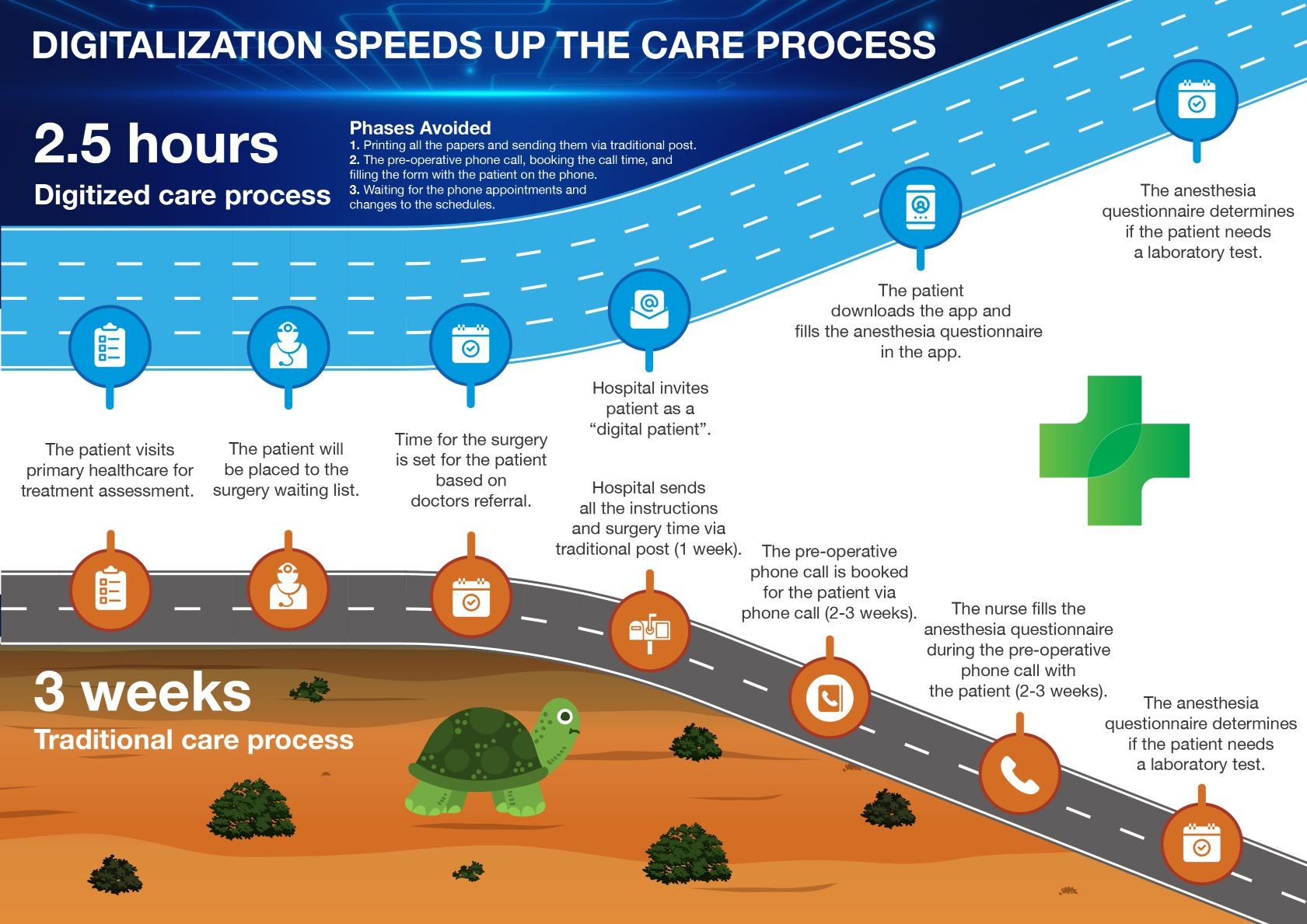
For example, by following a traditional surgical care pathway, the preoperative phase that includes the sending of instructions by traditional post, the booking of a pre-operative phone call, and the manual completion of the anesthesia questionnaire during the pre-operative phone call with the patient takes from two to three weeks.
In contrast, the same process is shortened to about 2 1/2 hours when a digital surgical care pathway is used. This is simply because most of these steps are automated and there's no need for phone calls or traditional mail to fill in assessments or give instructions to the patient. The quicker care pathway can be for example needed when preparing a new replacing patient for an operation after finding out a late cancellation.
This expediency is also not limited to the preoperative phase and can be just as valid in the postoperative phase. There's no need for phone calls to follow up with the patient to assist their recovery. Their progress of patients progressing normally can be monitored without an in-person consultation. The platform gives an attention notification when a patient having challenges in his/her care pathway. The triggers for attention notification are set by the care team when deploying the platform.
Apart from this, the automated task and appointment reminders and remote patient monitoring also improve patient no-show and late cancellation identification. This means that, because these patients are identified earlier and the process is so much faster, a new patient can be prepared for their surgery to take the place of the no-show. This, in turn, improves availability for patients and the facility’s profitability.
Final Thoughts about Digital Surgical Care Pathways
In order to improve the overall surgical patient flow, it’s necessary to optimize the surgical care pathway. With a digital surgical care pathway, facilities can design evidence-based workflows, and through the power of automation, can provide patients with an optimized care pathway.
If you would like more information on the BuddyCare Surgical Patient Management Platform, contact us today or visit our site for more details.