Surgery can be a daunting time for patients and seasoned medical practitioners alike. Patient-reported outcomes have long been used as a means of assessing patients' post-operative physical recovery. Still, the collection through traditional channels can be rather time-consuming, and a lack of proper reporting tools can provide challenges when making an analysis based on the patient data.
With healthcare systems across the globe facing increased strain, doctors, surgeons and hospital executives have been looking for new ways to help patients and collect outcomes and experiences data from patients while shouldering the burden of time limitations and out-dated traditional patient engagement strategies.
However, with electronic patient-reported outcome measurements (ePROMs), the future of patient-focused healthcare is bright. Electronic patient outcome solutions make the most of available technology and hospitals’ own administrative and caretaking procedures to reduce time wastage for healthcare practitioners by automated patient outcomes data collection and reporting while improving care for patients.
These strategies require a patient-focused, wellness-intensive approach to realize their full potential. With that in mind, we’ve created a list of 5 strategies to improve patient-reported outcomes in surgeries through ePROMs.
-
1. Switch from traditional to digital patient outcomes collection
Data collection is a key part of post-operative care. Medical professionals and patients alike recognize the importance of not just a post-op debrief session to indicate surgery success, but consistent, well-curated assessments to track recovery and deal with complications or unnecessary hospital readmissions before they become an issue.
Traditional means of collecting patient reports are by serial in nature, meaning a doctor, surgeon or hospital management can only process one patient’s report at a time and not be able to collect all patients’ data on one report. While this can already create time management and scheduling issues in smaller practices, it can have a stacked effect in larger hospitals with higher patient-to-practitioner ratios and more complicated procedures to inspect.
Switching to digital patient outcome collection allows patients to input their own reports into a well-structured system that facilitates the role of a healthcare professional sitting across from them. This allows multiple patients to input their data simultaneously or at times that are more convenient to them.
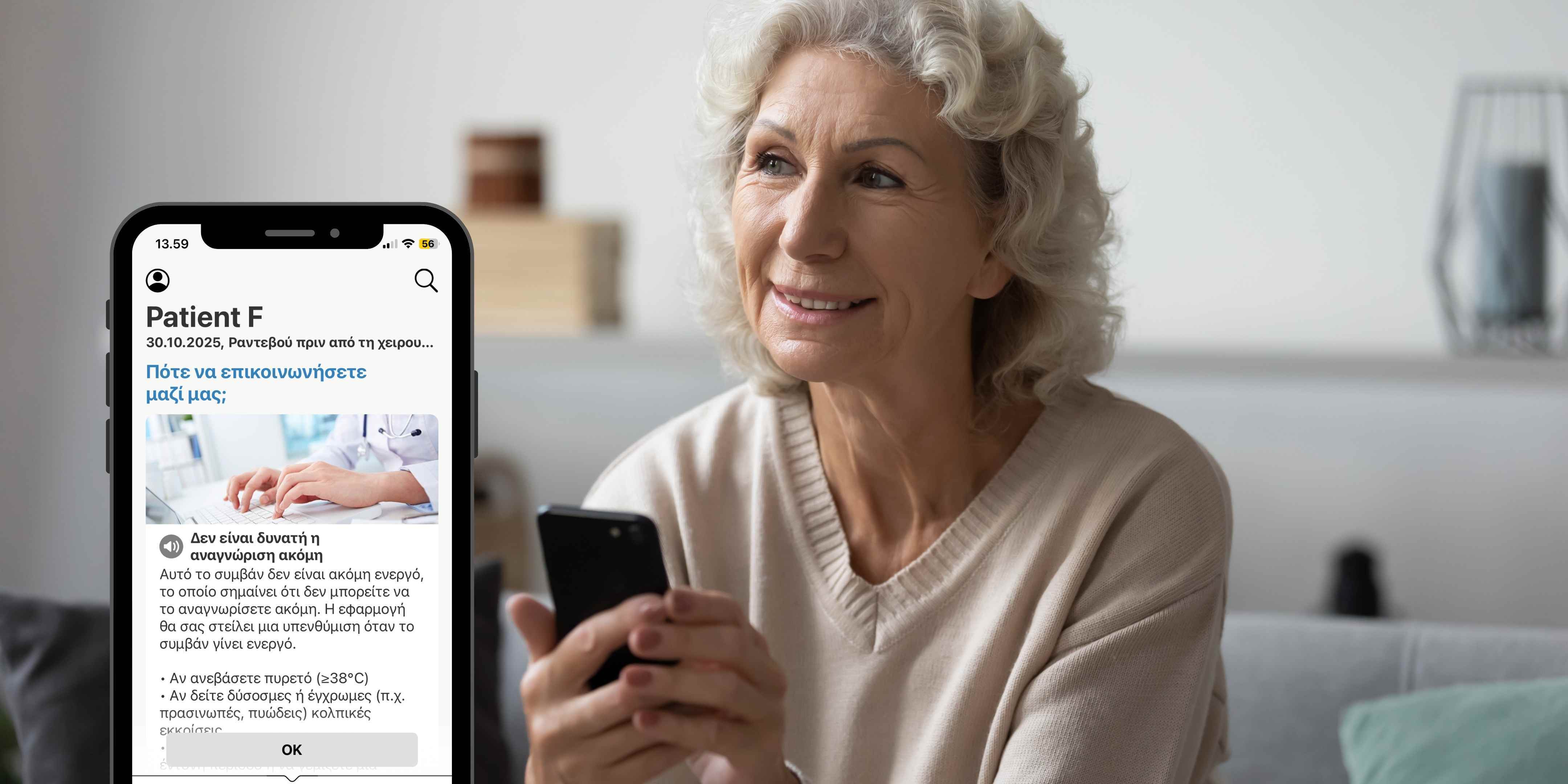
A proper all-in-one, digital patient engagement platform such as the BuddyCare Platform can help surgery clinics automate the patient outcomes and experiences (ePROMs, ePREMs) collection and reporting, simultaneously supporting the perioperative care coordination and patient management.
-
2. Refocus patient-to-practitioner engagement
Digital collection isn’t about removing the human factor in caretaking – it’s about digitizing time-consuming processes to allow medical professionals to focus on the areas where their human engagement is most needed.
Certainly, some time will be needed for healthcare practitioners to educate patients on how to use their digital systems, and this time should also be used to re-enforce how their emotional well being is still at the heart of these digital patient engagement strategies.
This is perhaps especially important in improving patient outcomes in nursing and other post-operative care. The benefits of ePROMs, however, aren’t limited to post-surgery patients.
-
3. Familiarise patients with the patient engagement platform and outcome reporting before surgery
Familiarising patients with the digital patient engagement platform the hospital uses before they undergo surgery can reduce the stress of learning a new system while in recovery. Patients who are already familiar with the technology can spend more time focusing on using it to aid their post-operative measures, and pre-op represents a good time to familiarise them with it.
As a touch of emotional well-being, this education process can also place a patient’s focus on the positive outcomes of their surgery rather than the procedure itself, and provide a sense of control and empowerment.
To reduce the stress of learning a new technology, we recommend that hospitals choose a digital engagement platform that is easy-to-use. For example, Buddy Healthcare's Care Coordination Platform is preferred by patients as it's user-friendly and easy to use. The patient-facing mobile App is available 24/7 in the patient's pocket, allowing patients to read educational materials and submit questionnaires at their own pace, when convenient for them. More than 90% of patients' use the App recommend it to other patients and according to the latest customer survey, more than 100% of healthcare professionals recommend it to their colleagues.
-
4. Create a pre-operative digital patient engagement strategy
Creating a space for ePROMs and ePREMs before surgery also opens up a new host of tools for digital patient engagement. Pre-operative patients will often be required to regulate their diet, sleeping habits, and undergo a certain level of mental preparation before the surgery.
Digital patient engagement platforms offer the convenience of automated reminders and push notifications straight to the patient’s mobile device of choice. This is a far more accessible form of scheduled communication as opposed to more traditional methods like in-person appointments, physical files and even email reminders that can often get drowned out in an inbox or rely on patients actively looking for them.
-
-
5. ePROM and ePREM Questionnaires and communication
Electronic PROMs and PREMs collection provides excellent platforms for hosting patient outcomes and experience reporting strategies, such as questionnaires. The best of them don’t just put the patient in front of a multi-answer screen, however, they actively educate and encourage patients as they report.
Lengthy questionnaires show a significant drop-off in patient engagement, so it’s advisable to structure questionnaires in such a way that they can be completed in 5 minutes rather than 15. Three short questionnaires spaced out over a matter of days are far more accessible than one lengthy questionnaire that might strain a post-surgery patient’s concentration and energy levels.
Spreading questionnaires out also allows doctors to track a patient’s progress by emphasising different stages of recovery with each questionnaire, while also providing patients with insight into their recovery phases.
Both ePROMs and ePREMs can be a great aid to hospitals that integrate the technology into their existing systems while creating usage strategies that focus on patient wellness, quality outcome reporting, patient experiences collection and digital efficiency
Read our blog here about how to automate the collection of patient-reported experiences (PREMs)?