Surgery can be one of the most daunting times in a patient’s life, and the same goes for the healthcare professionals tasked with bringing them through it safely and successfully. As difficult as it is to quantify the stress preoperative surgery can bring, the medical industry has always sought ways to mitigate it at every stage of the process.
Surgeries involve complex procedures that put unique physical, emotional and mental strains on patients. These strains continue even after a successful surgery is performed, as patients take time to recover.
The good news, however, is that there exists a system of strategies developed to care for patients at every single point of the surgical process, and it has a name – care pathways.
Patient care pathways have long been developed as a means to create safe and accommodating entry and exit strategies for patients undergoing surgery. Specifically, when we speak of the care directly before and after a surgery, what we’re talking about is perioperative care.
Given its importance, we wanted to answer some key questions surrounding perioperative care pathways today, starting with the most important one:
What is perioperative care?
As mentioned, perioperative care pathways refer to the strategies medical professionals use in order to prepare a patient for their surgery and to debrief and care for them post-operation. Perioperative care pathways are essentially the combination of preoperative, intraoperative and postoperative phases of care, but when combined, they create a more holistic approach to patient engagement.
Dietary monitoring (preoperative) and long-term pain management (postoperative) are usually adjacent care pathways that bookend perioperative care. Whether or not that care is provided by the same healthcare professionals who provide perioperative care often depends on the size of the hospital and its patient engagement capabilities.
The period in which perioperative care takes place also depends on the surgery, the patient’s conditions and circumstances, as well as the context surrounding the surgery. For emergency surgeries, the preoperative part of the care pathway tends to be much shorter, often limited to the key essentials required to prepare a patient.
For patients who have comorbidities and other conditions that might add complications, there is often more care required in the preparation phase, but the postoperative care can also be more intricate and thorough as a result.
What are the steps involved in perioperative care?
So given the holistic nature of perioperative care, it’s no surprise that it needs to be broken down into its core components to understand how the chain of care happens. Typically, perioperative can be broken down into three phrases. These phases, which we’ll discuss a little below, cover the necessary care on either side of the surgery as well as care during the surgery itself.
Preoperative care
Preoperative care describes the patient care strategies used in preparing a patient for their surgery. The length of this care period depends on what is required to successfully prepare a patient, and often, one of the most time-consuming elements of it is testing.
Because of the treatment and strain involved in surgery, healthcare professionals need to have a clearer understanding of the health benchmarks a patient is hitting before they enter surgery. This will often include medical analysis such as blood tests, scans, medical history and cardiovascular monitoring.
It will also require more hands-off assessments, such as dietary habits, surveys where patients can self-report and the psychological preparation required before going into surgery. Doctors and nurses both have roles to fill here, bringing their specialised skills to make sure all of a patient’s preoperative needs are met before they can be cleared for surgery.
Intraoperative care
Perhaps one of the most volatile times in the perioperative care pathways, intraoperative care is focused on patient safety during the surgery. In most cases, this care period starts when a patient is transferred to the operating room and concludes once they are transferred to the Post Anaesthesia Care Unit (PACU).
While a patient undergoes surgery, care is provided by the nurses and anesthesiologists charged with regulatory monitoring and all the vital peripheral tasks involved during surgery. Without these processes, a surgery cannot be successful.
Nurses will often be required to monitor vital signs, ensure that equipment is properly prepared and sterilised, prevent infection and place their focus primarily on safety.
Postoperative care
Postoperative care begins once a patient is transferred to the PACU following their surgery. This care period usually lasts until the patient is discharged from the hospital. It’s rare to find cases where the postoperative care continues past this point, and care is usually provided by a different group of professionals than the surgical team, who predominantly focus on preoperative and intraoperative care.
Why is it important to cover both preoperative and postoperative care pathways?
The importance of these care pathways cannot be overstated. Surgery comes with many obstacles, whether physical, emotional or financial. A patient needs to be in a state where they are calm and focused on their health rather than the surrounding issues of their situation.
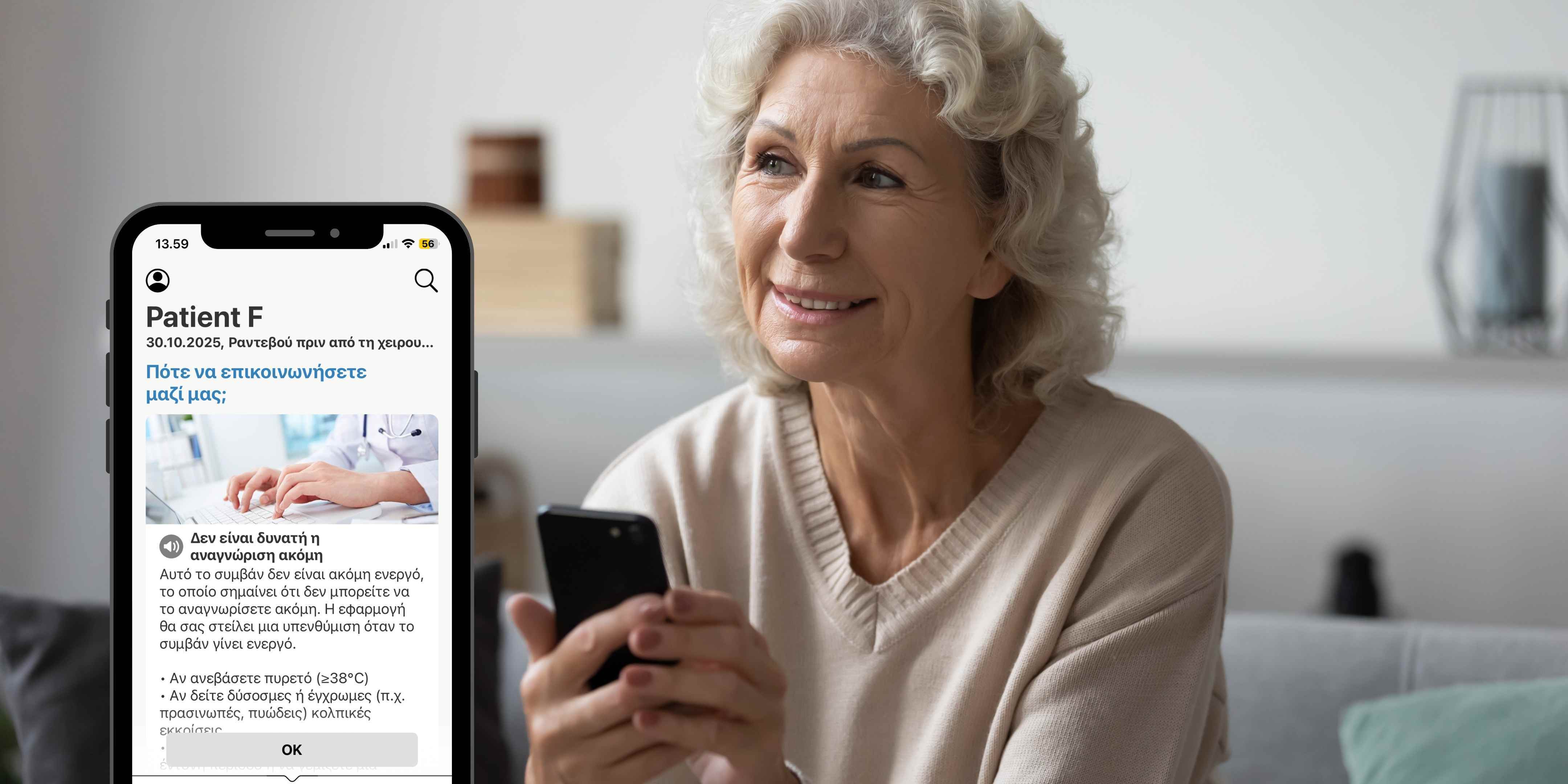
Digitised patient care pathways mean that patients can access the resources they need on their mobile devices. This provides additional benefits through the use of push notifications for automated care-related education, task and appointment reminders and online questionnaires and forms collection, such as automatic electronic pre-operative assessments collection.
Why should hospitals digitise entire perioperative care pathways?
Given the importance of patient care pathways, healthcare professionals are constantly looking for ways to streamline these strategies. The introduction of digitised patient engagement platforms have allowed doctors and nurses to collect data more efficiently, while also creating a greater degree of accessibility for patients through remote monitoring.
Digitised patient care pathways mean that patients can access the resources they need on their mobile devices. This provides additional benefits through the use of push notifications for automated care-related education, task and appointment reminders and online questionnaires and forms collection, such as automatic electronic pre-operative assessments collection.
Additionally, in the post-operative phase, hospitals can collect pain scales from patients, share post-op exercises in video or text format, share post-op medication or wound care instructions, collect patient outcomes and experiences questionnaires, and monitor patients’ progress or activities remotely. All these steps can be implemented digitally without the need to do manual work.
Today’s digital health solutions, such as Buddy Healthcare's care coordination, can automate entire perioperative care pathways care coordination, reducing care personnel workload and cost significantly. At the same time, digital solutions can offer tools to identify potential no-shows and cancellations earlier and help in preparing to replace patients faster and more easily.
As complicated as the marriage of the digital world and medicine may sound, both industries have the same goal when it comes to patient care – to simplify the process for patients and to make it more efficient for healthcare professionals.
Do you want to learn how the Buddy Perioperative Care Coordination Platform works? Check out our Platform page or simply get in touch with us by sending us your question through our contact form, and our team will get back to you promptly.