CARE COORDINATION SOFTWARE TO OPTIMIZE SURGERIES
Automate your patients' perioperative care pathways and improve your hospital’s operational efficiency with care coordination software.

Improved hospital outcomes
98%
fewer pre-operative phone calls
50%
fewer no-shows/cancellations
20%
reduction in patients' post-op visits
>90%
of patients recommend the app
Automate and manage your surgery patients' perioperative care pathways
BuddyCare Care Coordination software enables hospital surgery care units in automating their care coordination and patient communication processes. The care coordination software helps care teams keep accurate records and track patients - from the beginning of their surgical care pathway to recovery.
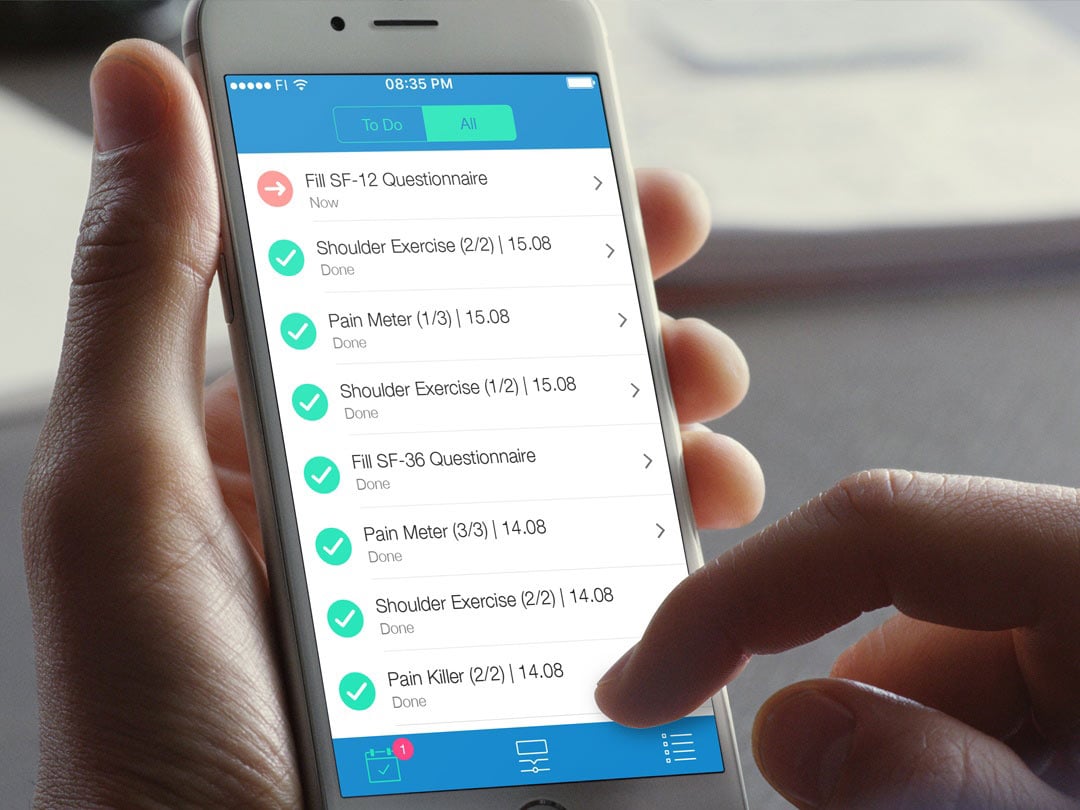
Patient-facing app for your patients
Patients preparing themselves for surgery use an app to receive care-related timed information, instructions, and tasks from the hospital. The patient communication process is fully automated for the hospital, and the care coordination software collects electronic pre-assessment forms or in-app questionnaires such as PROMs/PREMs from the patients.
After surgery, your patients receive all post-operative instructions and rehabilitation exercises conveniently on their app. Patients can also submit their pain scales, PROMs and PREMs through the app. Timed and automated digital postoperative support help in identifying potential postoperative complications, thus reducing hospital readmissions or length of stay.
The entire patient communication process is automated, but if needed, care teams can provide patients personalised care through secure messaging.
” The app relieved my tension and uncertainty before the surgery.”
- Patient
Efficient patient management through clinical monitoring dashboard
Our care coordination software enables the care team to monitor and manage patients' care pathways. Through the dashboard, care providers have a real-time 360 degrees view of all of the patients' care pathways and activities. The care coordination software provides a quick and easy at-a-glance overview of the patients' care progress. The dashboard provides attention notifications if a patient is about to deviate from the care pathway or the patient's condition deteriorates helping healthcare providers to intervene sooner at early signs of potential no-shows, cancellations, or other identified challenges such as postoperative complications.
Automate PROMs and PREMs collection
The care coordination software automates patient-reported outcomes and patient-reported experiences collection. Patients can submit easily their answers from the app, and the dashboard collects the questionnaires and produces reports for care team analysis. Read more from our blog on how to automate PREMs or PROMs collection.
“The automated instructions and patient reminders make it easier for the patient to prepare for surgery, and they have reduced our last-minute cancellations. In the post-op phase, the patient can send an image of the surgery wound for our surgery team through a secure messaging feature, and we can assess the healing remotely, thus reducing unnecessary post-operative visits to the hospital.”
- Day Surgery Nurse, Central Hospital


Our care coordination software can help to improve surgery clinics' operational efficiency such as:
- Automate pre-and post-surgery care coordination and communication → fewer phone calls, less paperwork;
- Improve cancellation/no-show identification → cost and time savings;
- Provide more efficient new patient scheduling after cancellation;
- Improve patient safety and unnecessary cancellations with pre-op health screening;
- Interact with the patients through care coordination software instead of calling;
- Automate all forms and in-app questionnaire collection and reporting.
Automated Care Coordination with the BuddyCare Platform
Mobile App for Patients
The patient-facing BuddyCare app helps patients to navigate through their care pathways.
Timed reminders and push notifications ensure that patients get the right information at the right time.
Patients can submit forms or in-app questionnaires to the care personnel and interact via the mobile app.
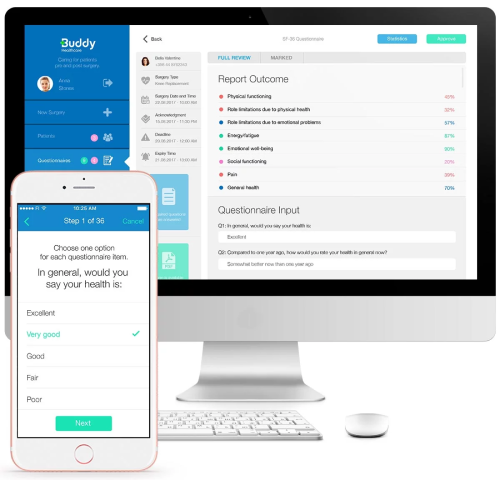
Dashboard for Care Personnel
With the dashboard, the hospital care personnel can monitor patients' care progress and see at-a-glance if patients have read all education, submitted in-app questionnaires and followed all instructions
The dashboard collects data during the patients' pathways and enables patient interaction. The dashboard produces reports for analysis.
