There are many ongoing discussions about clinical pathways (also known as care pathways and integrated care pathways) and what to consider when producing them. Clinical pathways are evidence-based road maps that assist in reducing variations in clinical practice (Hipp et al., 2016). The pathways act as some of the most important tools in maintaining high-quality healthcare by standardising care processes.
Clinical pathways emerged in the literature in the early 1980s, and the term was rather different from how we use it today. However, the basic principle is still the same: execute best practices for care delivery workflow with established time frames.
These goals are ambitious, but what must one do to create these care pathways?
In our experience, here are a few ideas to start with:
- Baseline and mapping
Are there standardised care pathways for certain patient groups already in place? How effectively are the pathways executed? Was the baseline data collected at the beginning of the pilot project? What variables need improvement? At first, everyone should analyse where we are at, why improvements are needed, and what needs to be achieved.
- Interdisciplinary teams: Since various healthcare professionals care for the patient during the care path, the medical staff should contribute to creating a consistent workflow.
- Process leaning: What inconsistencies, unnecessary steps, or other poor resource allocations have been discovered in the care path? Knowing this, we can develop key performance indicators that will help us.
- Piloting: Compare the baseline data about the patient to the data collected during the pilot phase. For example, how long did the patient spend at each stage of the treatment process, and how has this changed after the beginning of the pilot project? Variance analysis can be used as a tool. How do the results deviate from the expected care path and why? Based on the analysis, we can make further improvement plans.
- Go / No Go: Were the results satisfactory, or is there room for more improvements?
There is not much literature on how to develop successful care pathways at the moment, but Great Ormond Street Hospital for Children in the UK discusses similar phases.
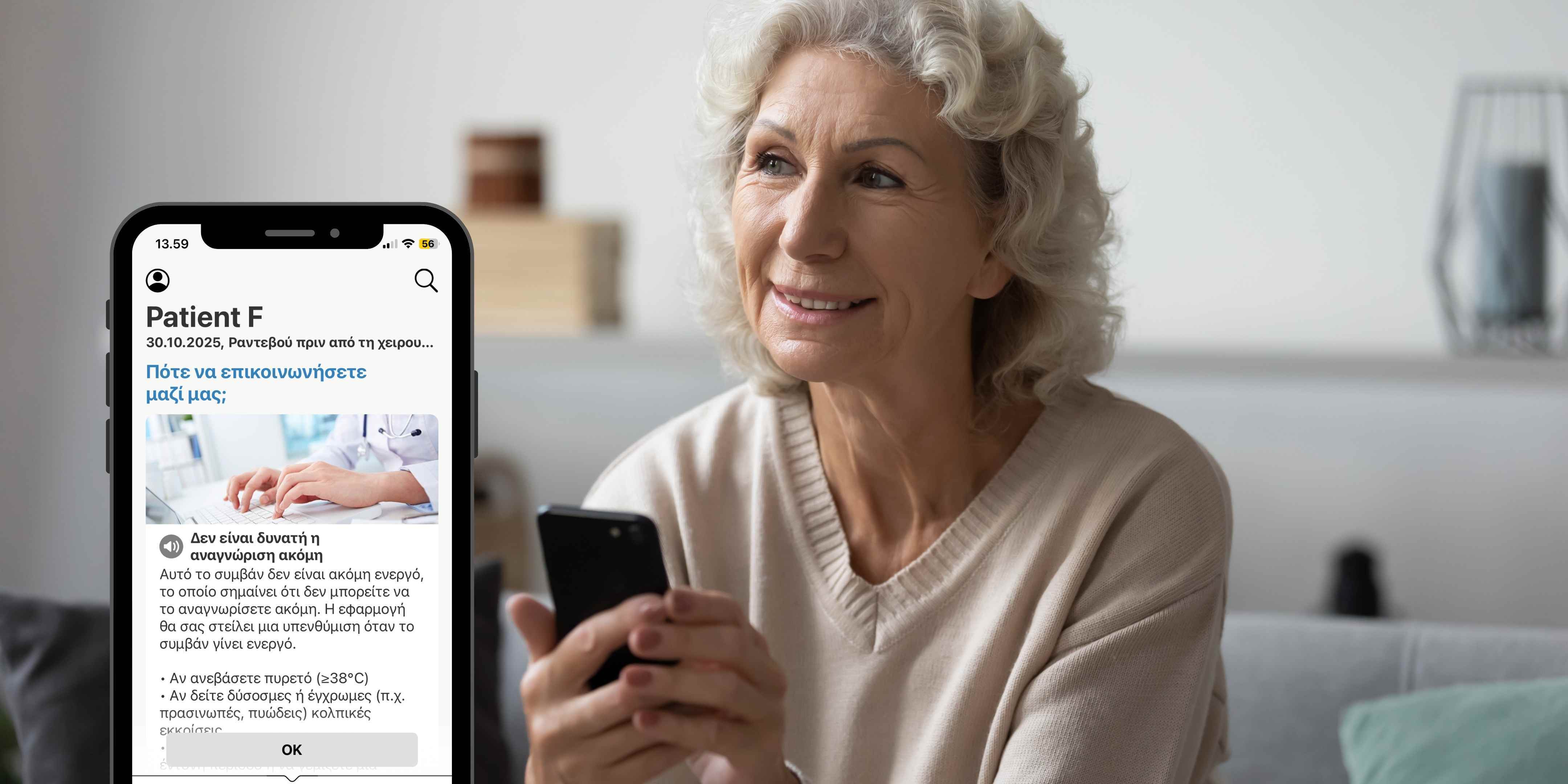
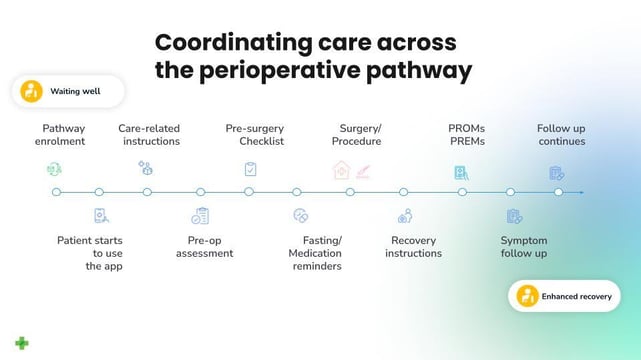
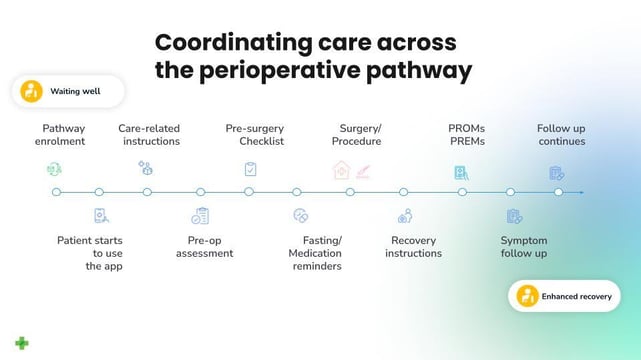
These are the principles we found that work. Our customers, several hospitals and care providers across Europe, use our Care Coordination Platform to make care paths mobile for patients and to automate care coordination for hospitals. This has enabled us to gather data on how patients stay on track on the care path, acknowledge instructions, and carry out other essential tasks during the pre- and post-operative phases, thus making improvements based on the collected information.
Clinical care pathways
Understanding how care pathways are integrated into various healthcare systems is vital for understanding what tools and practices are available to hospitals and their patients. Because healthcare facilities rely on creating evidence-based pathways tailored to a specific patient's needs, the available options need to be understood.
To better understand how these pathways work, we can look to real-world examples of how they’ve been implemented in modern healthcare.
Liverpool Care Pathway for the dying patient
Also known as LCP, the Liverpool Care Pathway for the Dying Patient was a care pathway developed in the United Kingdom. Since its introduction in the late 1990s, the pathway has sought to cover palliative care options for patients in their final days of life.
Proceeded by a less standardised model of end-of-life care, the LCP was developed to help doctors and nurses provide quality end-of-life care for dying patients in the UK.
Developed by the Royal Liverpool University Hospital and the Marie Curie Palliative Care Institute, the initial public reaction to the LCP was generally positive. However, the pathway came under intense criticism between 2009 and 2012 when it was enacted by the Liverpool Community Healthcare staff.
Following this, the Department of Health elected to phase out the LCP over the next year (2013) and replace it with the current active pathway, an “individual approach to end of life care for each patient.”
Surgical care pathways
Surgical care is a little different to clinical care pathways. For one, surgical care pathways are generally broken up into five phases:
1) Preoperative
The processes administered in or occurring before the surgery to prepare a patient
2) Perioperative
The process or treatment that is performed at or around the time of an operation
3) Intraoperative
The process occurring or performed during a surgery
4) Postoperative
Related to processes that occur following a surgery
5) Post-discharge
The processes that are enacted once a patient is discharged from the hospital following surgery
Understanding these different phases of surgery is important because surgical care pathways are created to address every point in the surgery cycle.
The American College of Surgeons (ACS) believes that registry-based quality measures that account for every phase in the surgical care pathway may be the future of surgical care. Of course, this is when a five-phase plan includes coordination between doctors and their patients to help meaningfully fit the pathway structure around a patient’s needs.
This communication and collaboration involves doctors walking patients through each phase of the surgery, ensuring that they clearly understand the processes involved and how best to prepare for them mentally, emotionally and physically.
Because of the complexity of five-phase surgical care pathways, there is an ever-increasing need to provide a framework that patients can understand to reduce stress and help them engage with it productively.
The ACS began integrating patient-reported experience measures (PREMs) in 2018, and it has focused on measuring the goals of “high-quality, patient-centred surgical care.
If you wish to learn more out more about Buddy Healthcare's care coordination solution for automating surgical care pathways, please visit our platform page and get in touch. Thanks for reading, and until next time!