Elective care waiting lists: a growing problem.
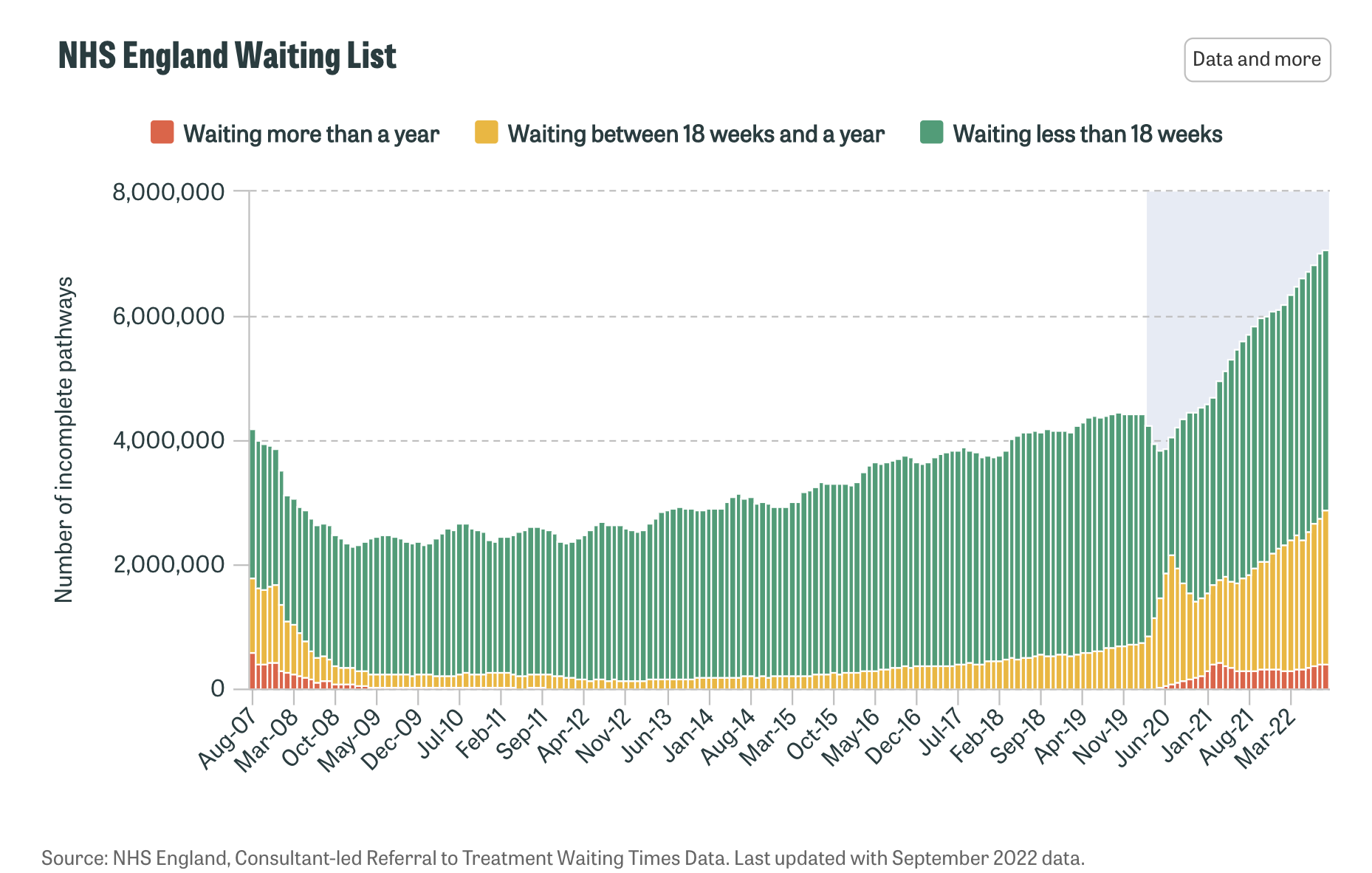
The number of people waiting for NHS treatment in England rose sharply as a result of the Covid-19 pandemic, with NHS England reporting 7.1 million incomplete treatment pathways in September 2022.
Meanwhile, according to Public Health Scotland, more than 750,000 people were waiting for an outpatient appointment, key tests, or hospital treatment.
Patients are facing increased delays at almost every stage of their NHS treatment, as the health system struggles to find the resources to deal with demand.
The data from September shows waiting lists across England have surpassed record highs every month for two years running, one of many major challenges currently facing the NHS.
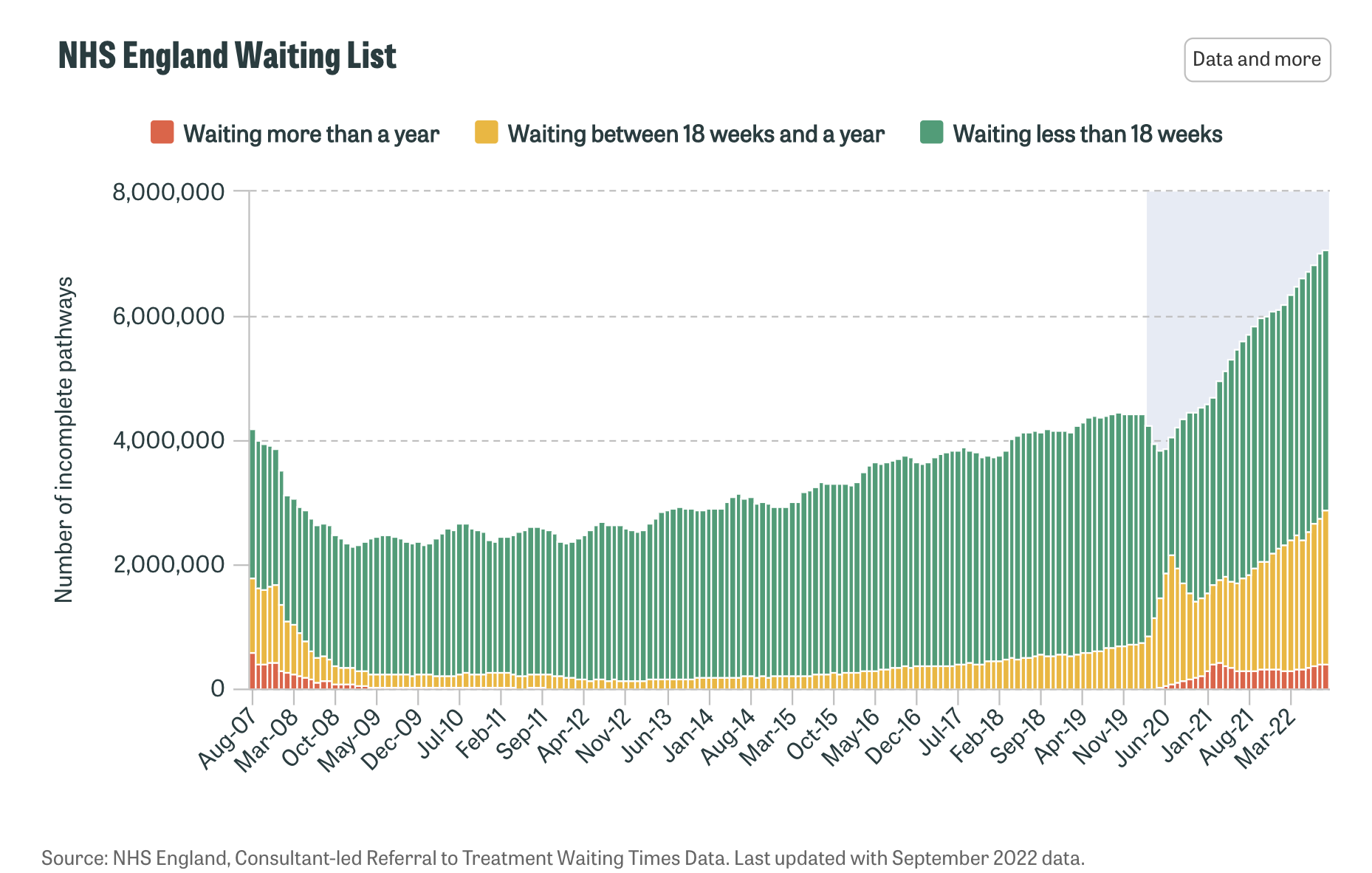
Source: NHS England (September 2022 data) – the graph shows the NHS waiting list since comparable records began in August 2007. It shows a particular rise in the number of people waiting more than 18 weeks, the NHS waiting target.
Latest official figures from December 2022 are showing that the waiting lists in England for non-urgent care in hospitals have reached a new record high of 7.2 million people. Of those, 410,983 had been waiting for more than a year for treatment, such as a hip or knee replacement, cataract removal or hernia repair – that should take a maximum of 18 weeks.
A government-commissioned paper by the King’s Fund health think tank stated that, by addressing shortages of health care staff and physical resources urgently, it would bring opportunities to reduce waiting times in the present day.
In this article, we are looking for ways to support staff shortages by adding efficacy to the care coordination processes and waiting list management by incorporating automation into the existing traditional labour and admin-heavy care coordination.
Recognising the role of technology.
The NHS is actively embracing the use of technology to help health and care professionals and enable citizens to access the care they need quickly and easily when it suits them.
Pre-dating the Covid-19 pandemic, the NHS published its ‘Long Term Plan’ on 7th January 2019. The plan set out its ambitions for improvement over a ten-year period. It underpinned the importance of technology in the future NHS, setting out the critical priorities that would support digital transformation and provide a step change in the way the NHS cares for citizens.
It was an approach that would see the service embrace digital, from websites to apps, that make care and advice easy to access, connecting to systems that give results, history and evidence to allow care teams to make the best decisions for patients, working smarter and ultimately providing better care than ever before.
Digital platforms that bring care coordination and automation to the services that the NHS provides can help with staff shortages and enhance patient communication, data collection and triaging during the wait.
What role can a digital patient pathway play in easing NHS pressures?
A digital pathway can redefine what a surgical pathway should look like. Digital pathways can be moulded around the patient, with the ability to avoid unnecessary physical appointments, late cancellations, Did Not Attends (DNAs), and support with recovery and remote patient monitoring. It can form an effortless communication link between home and hospital.
Recognising the pressing challenge of mammoth waiting lists, hindered by outdated, paper-heavy systems, and having the support to embrace proven digital technologies that can ease the elective surgery and care backlog burden is key to change.
Hospitals have to have regular contact with patients on waiting lists – that’s a reality that will never change; however, the manner of that contact can.
A digital platform can tackle the waiting list challenge through automated patient education, patient data collection and providing care teams with a single view of the patients' progress and status. These growing issues can be facilitated with hospitals being able to digitise waiting list management and triaging processes with a digital care coordination and care pathway management platform.
It means they can modernise and optimise surgery waiting list management, whether that’s by automating patient communication and data collection during the pre-operative phase, or education on keeping as fit and healthy as possible.
While the pandemic exacerbated the pressure on the NHS and many other public services, it facilitated a move towards embracing more digital services. It provided an opportunity to create a more inclusive, flexible, and accessible system.
These advances can be applied to an “end-to-end” approach, resulting in better patient outcomes, cost savings, increased efficiency and hospital capacity.
The impact of digitising pathways can be seen through statistics collated by Buddy Healthcare:
.png?width=2103&height=1265&name=map%20buddy%20(1).png)
By digitising a process such as this, care teams can drive down preoperative phone calls by as much as 98% (Buddy Healthcare, 2022) and significantly reduce the time spent per patient, especially in the preoperative phase. In addition, it can drive significant cost savings:
.svg)
Filling surgical slots by identifying flexible patients
Digitising care pathways is more than just reducing paperwork and freeing up time; it also means opportunities can be maximised and expedite other waiting list issues. One patient’s inability to have surgery can be another’s opportunity.
A digital care pathway management platform can, for example, help hospitals to fill surgical slots caused by late cancellations.
By reviewing patients' submitted and viewed data, care teams can quickly and easily identify fit patients ready for surgery at short notice to fill cancelled surgery slots. This digital pathway supports efforts to tackle backlogs of elective surgeries postponed with an efficient preoperative process and helps to optimise operating theatres.
Case study: how we worked with NHS Lanarkshire to support the innovative delivery of care pathways.
Working with Buddy Healthcare, NHS Lanarkshire hospital Board launched “Elsie”, an ePreOp digital platform. It was designed to replace the previous resource-heavy “paper-based” system, which required every patient, no matter their fitness for surgery, to attend a hospital appointment to answer questions with a nurse.
As part of Elsie’s rollout, while preparing for their surgery, pre-operative assessment patients are now guided and educated through a preoperative care pathway via a white-label mobile application called Elsie. The process helps the Health Board hospitals to identify patients who don't need to come on-site, reducing the clinical time required per patient and increasing workforce efficiency. This supports the effort to make surgery waiting list management more efficient by automating patient communication and providing data collection during the patient journey.
Patients use the app to:
- Access specific hospital-based information, i.e when arriving for surgery, how to find the surgery unit, or where to park
- Receive pre-habilitation information to inform the patient about “keeping fit for surgery”
- Use in-app two-way communication to allow the patient to ask questions, advise of a change of circumstance and for Staff to provide information in reply
- Automated care path instructions and reminders, i.e. fasting and medicine reconciliation details
- Receive clearly communicated updates on any changes to events
- Provide feedback and influence service improvements
Care teams use the clinical dashboard to:
- Manage and monitor patient engagement throughout the patient care path and outcomes
- Assess and triage the patients via the Elsie app care path to see if they are “fit for surgery”
- Work more flexibly - any location
- Remote patient monitoring and assessment
With Buddy Healthcare's electronic preoperative assessment platform, the surgical teams in three NHS Lanarkshire hospitals now remotely assess and monitor patients' progress and surgical readiness. The care teams use the clinical dashboard to gather and visualise patients' submitted health data. The clinical dashboard allows the care teams to manage a clinic or department of patients and monitor progress. It notifies of incomplete tasks or reduced engagement when necessary.
The digital solution enhances preoperative assessment clinic efficiency, optimises waiting list management, reduces unnecessary preoperative hospital visits, and allows patient care at the right time and place.
How to get started?1. Need more information?
Did you want to learn more about optimised waiting list management or a digital preoperative assessment process? Please check out our resources on waiting list management and the electronic pre-operative assessment process.
2. Prefer to watch an overview?
Do you prefer to see a few minutes of an overview video on how our care coordination platform digitises and automates the entire perioperative care process? You can access the video here.
3. Want to see our care coordination platform live?
We would love to hear from you. Feel free to get in touch with us and book a meeting.
We will use the meeting time to evaluate your current care processes, understand your interests and needs, and discuss how Buddy Healthcare may be able to improve your care coordination processes, including a more efficient waiting list management process.




.png?width=2103&height=1265&name=map%20buddy%20(1).png)