The white paper is based on the Master's thesis study: Alén, M., LUT University, Finland, 2022
An overview of the key results
The white paper presents the following and time and cost-saving results of the economic effectiveness of a coordination platform in the care process of ear-nose and throat disease surgical patients in Satasairaala Hospital in Finland.
- The implementation of the care coordination platform reduced the cost of care for surgical patients in the units studied by significantly reducing the number of nurses’ appointments.
- The care pathway analysis found cost savings ranging from €39.7 to €91.6 per patient, with net benefits exceeding costs.
There is a growing need to increase the economic and process efficiency in healthcare.
The social services and healthcare environment is under enormous pressure to change. Despite systematic development of the service system over the last few decades, the public sector is facing major challenges with rising demand for the services and increasing costs.
There is a great need for developing healthcare provision with additional pressure from digitalisation and technological development, which necessitate the review and assessment of the processes related to social services and healthcare. While all healthcare aims to promote the health and well-being of the population, both economic and process efficiency should also be considered in the provision of services to ensure sustainable development and the sustainability of the healthcare system.1
Not all digitally-led improvements to healthcare are measured accurately.
Evidence suggests that digital solutions can improve healthcare efficiency and reduce care costs, which corresponds to the necessity of improving the health service system. However, shortcomings have been found in measuring the cost-efficiency of activities, even though a number of ways to improve cost management have been identified.
Providing evidence of the economic effectiveness of digital solutions is, therefore, a hot topic in the health technology industry, as evidence is needed in support of the potential of new approaches to contain costs in the health service system, streamline care pathways, and improve productivity and efficiency. 2
The rising need for a more detailed analysis of its economic effectiveness and economic benefits
Buddy Healthcare is a Finnish health technology company that digitalises and automates healthcare processes. The company’s care coordination platform was created in collaboration with several university hospitals to provide solutions for more efficient and clearer coordination of care pathways. The care coordination platform is currently used in several university hospitals, central hospitals and private clinics across Europe, in 25 different medical specialities. The increasing use of the platform has raised the need for a more detailed analysis of its economic effectiveness, demonstrating its benefits and calculating the cost savings it can achieve.
As the topic is current and important, the economic effectiveness of the care coordination platform was investigated in a recent thesis study carried out in collaboration with Wellbeing Services County of Satakunta Hospital, a client of Buddy Healthcare. The study aimed to evaluate the cost savings achieved through improved operational efficiency and to demonstrate the economic benefits gained in the digital care pathway of surgical patients from the hospital’s perspective. Examining the care pathways focused on outpatient clinics and the preoperative phase of the care process.
Methods used
The data was collected using collection methods for qualitative and quantitative data in the Ear, Nose and Throat (ENT) Unit and the Gynaecology Unit of the Satasairaala Hospital. Both have Buddy Healthcare’s care coordination platform in place. The results were compiled from staff interviews and care pathways of surgical patients modelled on the basis of the interviews, statistical data on the number of users of the care coordination platform, cost data on nurses’ appointments and a comparison of the costs of different types of appointments. In this white paper, we present the Ear, Nose and Throat (ENT) Unit’s study findings.
Study results: Economic effectiveness of the care coordination platform.
Digital solutions in healthcare are often expected to be economically effective as they are expected to improve the efficiency of the operations and bring cost savings. Expectations may be focused on, for example, reduced service utilisation by patients, lower service costs or improved workflow for the staff. However, measuring the effects of digital services is a complex process. Therefore, a systematic and comprehensive evaluation is challenging but essential to demonstrate effectiveness.3 The data from the study enabled the examination of the economic effectiveness of the care coordination platform in a holistic manner. The benefits of the implementation of the care coordination platform, as well as the resources used to achieve them, were measured and evaluated.
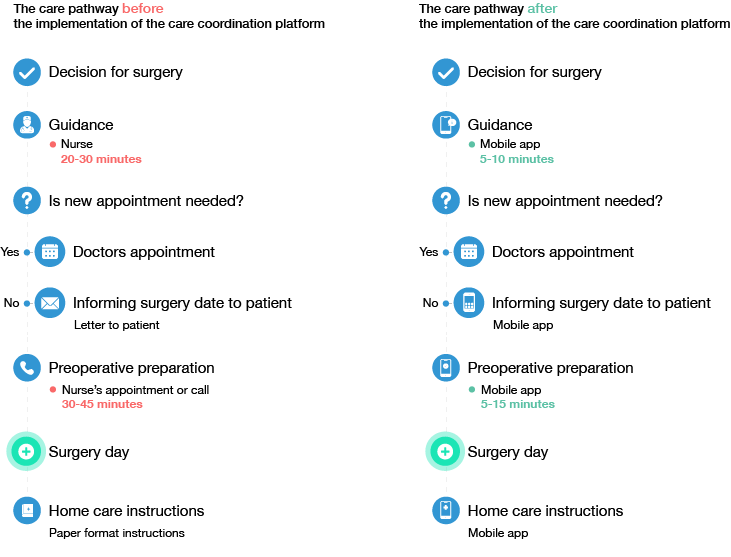
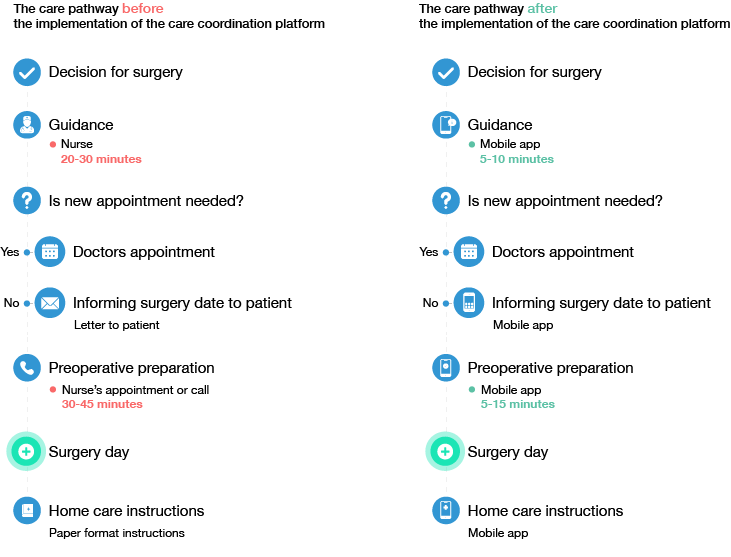
In the study, changes in the care pathways of surgical patients were modelled on the basis of staff interviews. The care pathways before and after the implementation of the care coordination platform were then compared. The interviews focused on the lead time of the care pathways, based on staff estimates of the workflow and the time taken by nurses to complete the different work phases.
The modelled care pathways were also used as a basis for assessing the cost effects of the care coordination platform. The assessment also utilised information on the number of users within the care coordination platform and the cost data from the hospital’s service price list. The aim was to assess whether the implementation of the care coordination platform resulted in savings and whether the activities were economically beneficial. The focus was on the replacement of conventional nurses’ appointments with the care coordination platform.
Study findings: The platform had a wide range of economic effects on the care process of surgical patients.
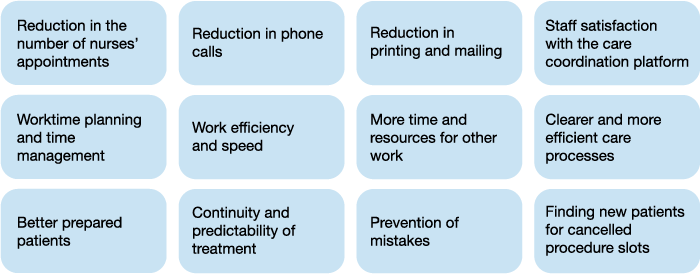
The thesis study found that the care coordination platform had a wide range of economic effects on the care process of surgical patients, with the platform being economically beneficial in terms of costs and effective in terms of operational efficiency.
- The implementation of the care coordination platform reduced the cost of care for surgical patients in the units studied by significantly reducing the number of nurses’ appointments.
- The care pathway analysis found cost savings ranging from €39.7 to €91.6 per patient, with net benefits exceeding costs.
- The care coordination platform also helped to improve the planning of staff working hours and time management.
- Just by moving appointments to the care coordination platform, thirty to sixty minutes of nurses’ time was spared per patient per care pathway.
- It was possible to use the saved time and resources, for example, to treat other urgent patients, as the number of preoperative appointments for patients coming in for surgery reduced.
A cost estimate of the care pathway for an ear, nose and throat surgery patient.
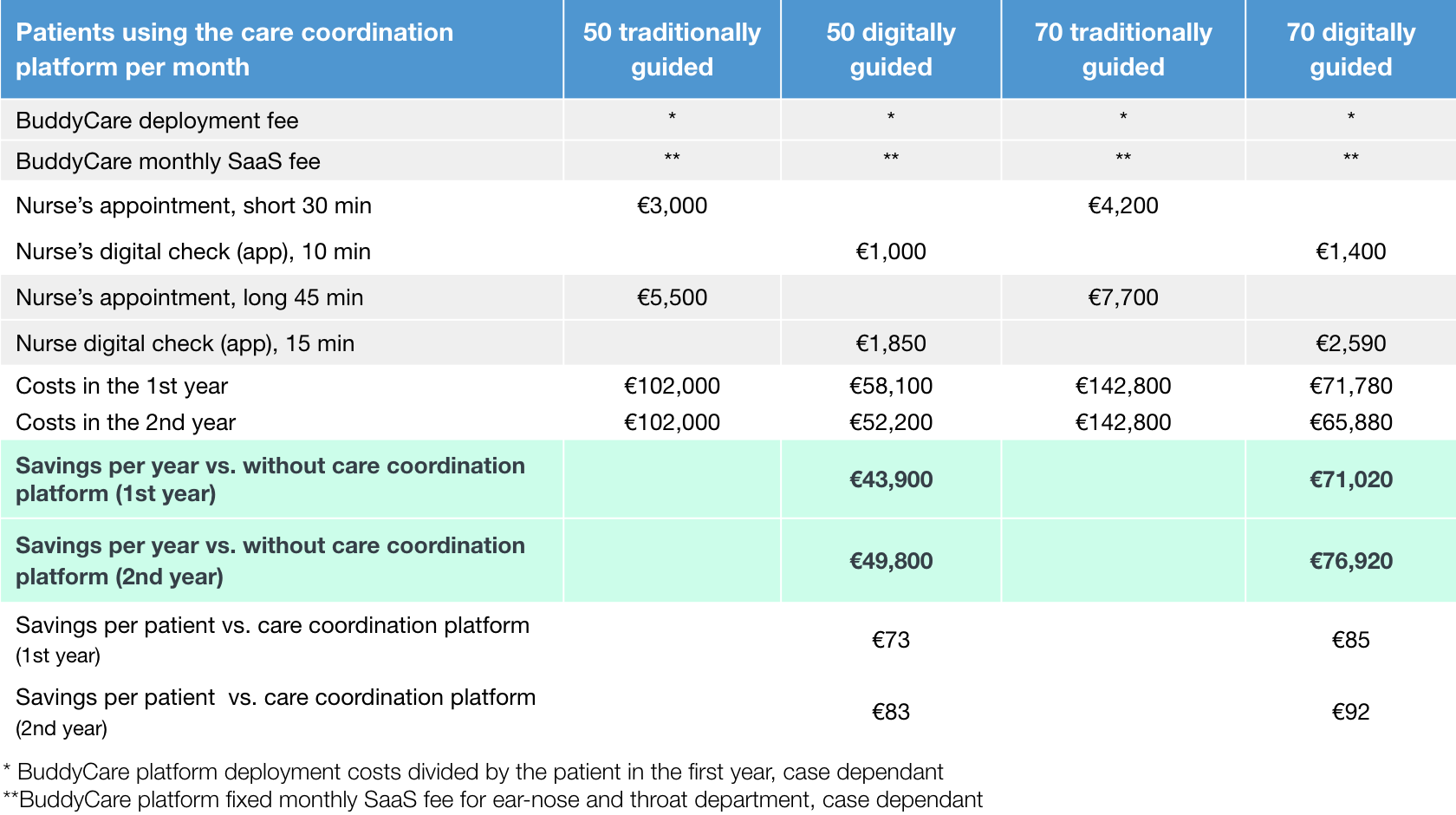
In the following, a cost estimate of the care pathway for an ear, nose and throat surgery patient is presented as an example from the study. The costs used in the cost calculations carried out for the study are based on the hospital’s service price list (2022).
The cost of nurses’ appointments included all overheads and administrative costs. Therefore, the prices represented the actual total cost to the hospital of a single type of appointment. Based on the interviews and the modelling of care pathways, appointments with nurses were defined as short appointments (20–30 minutes) and long appointments (30–45 minutes). Pre-arranged telephone appointments arranged instead of a nurse’s appointment were also counted as nurse’s appointments.
The care pathway modelling showed that, on average, the use of the care coordination platform could eliminate one short and one long appointment for an ear, nose, and throat surgery patient.
According to the hospital service price list, a short outpatient appointment with a nurse in the specialist field of ear diseases costs the hospital €60 per appointment. In contrast, a long outpatient appointment with a nurse costs the hospital €110 per appointment.
A cost was also calculated for the replacement of appointments with the care coordination platform, which included overheads and administrative costs. The time and cost of the appointments were compared with conventional appointments. In addition, the study included the units’ customer-specific initial investment and operating costs resulting from the use of the care coordination platform per patient, allowing the analysis of the economic benefits of the platform and its actual net benefits at various patient volumes.
Cost calculation of the care pathway for an ENT surgery patient for two different patient volumes (50 and 70).
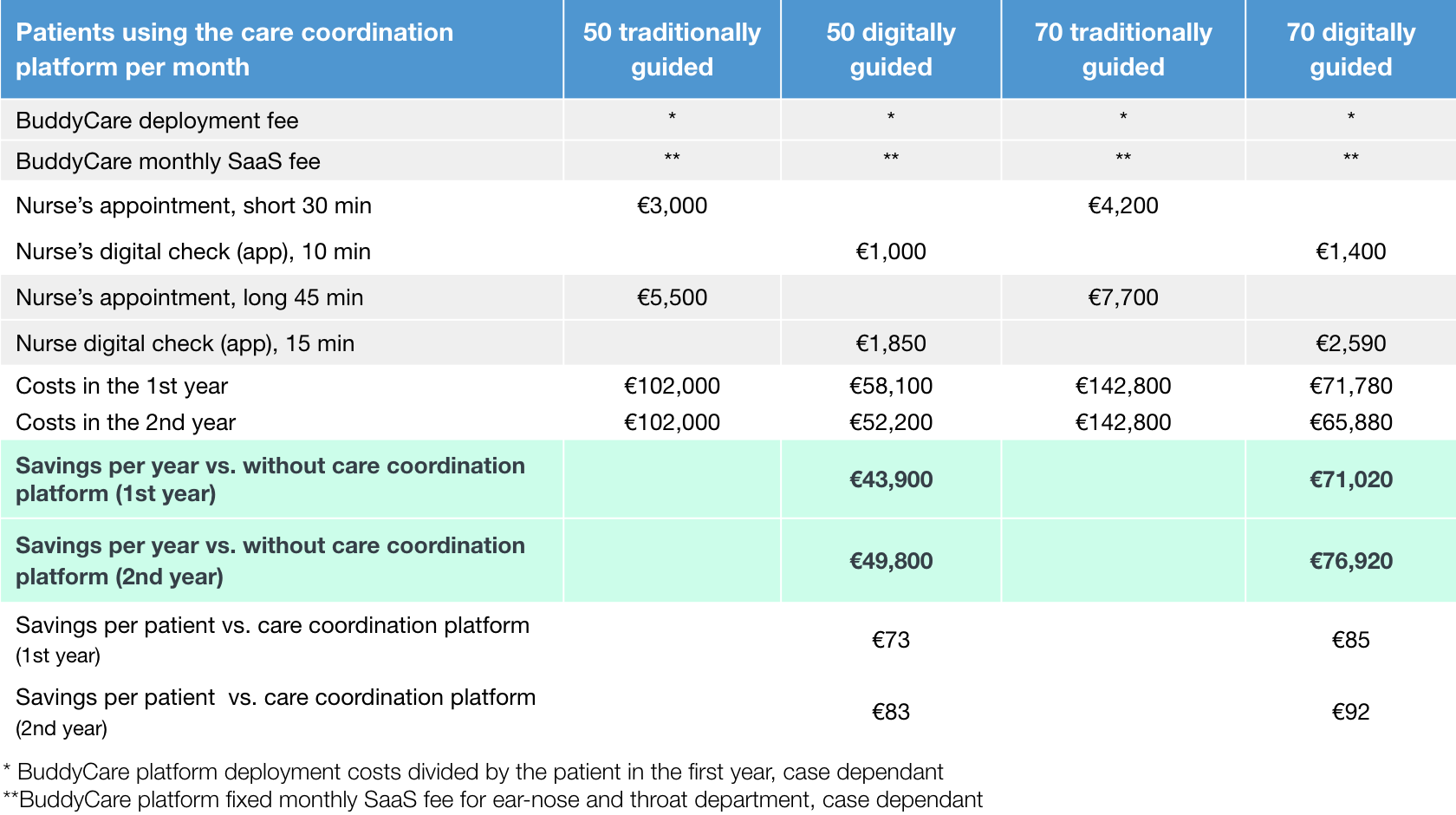
Cost calculation of the care pathway for an ENT surgery patient for two different patient volumes (50 and 70). Savings are reported in the first and second years, as the initial investment in the care coordination platform was spread over the first year. In the second year of operation, the cost of using the platform decreased.
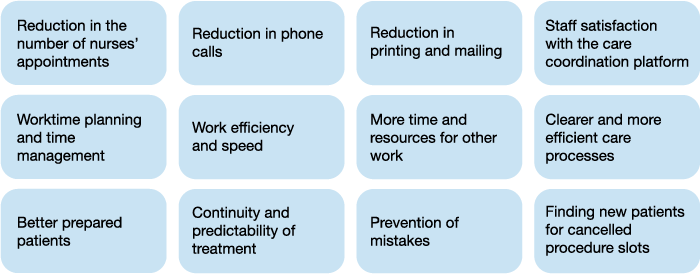
The study measured the preoperative economic effectiveness of the activities in terms of cost savings and time savings based only on changes in nurses’ appointments. However, the calculation of costs is only one aspect of economic effectiveness, as a smoother workflow, perceived staff satisfaction and more efficient working practices are also benefits and have an economic value, even if this value is more difficult to quantify in monetary terms. Additional savings from patient-related DNAs and readmission reductions are expected with digitally guided patients.
The study was able to demonstrate the efficiency of the care pathway for surgical patients, and the benefits resulting from the implementation of the care coordination platform were demonstrated not only through cost calculation methods but also by staff interviews.
Economic benefits of the care coordination platform.
Conclusions
From an economic point of view, the aim is to improve productivity and efficiency and to keep costs under control. While monetary savings from more efficient service provisions are an essential objective of cost-effectiveness, economic effectiveness also comprises solutions that are better in terms of saving time and improving resource allocation. The benefits of the care coordination platform can also be considered to have a broader societal relevance, as there is a need to develop the efficiency of care processes and cost containment within the public healthcare sector nationally to ensure the financial sustainability of the publicly funded service platform.
Buddy Healthcare’s care coordination platform does more than merely reduce the costs of care for surgical patients, as mere cost savings can also be considered to reduce the efficiency of the activities. For example, if costs are controlled by simply reducing the allocated resources, the efficiency of the process in question may suffer, increasing the costs in the end.4
In contrast, the care coordination platform reduced costs by genuinely improving the efficiency of the activities and making the work easier for staff, with the value of the benefits exceeding the value of the inputs. This is precisely the essence of the economic effectiveness that the implementation of the care coordination platform achieved in the care process of surgical patients in the units studied.
More information on the thesis study.
The thesis has been published in LUT University's open-access archive. It describes the economic effectiveness of healthcare in a broader context and presents the full study results (staff interviews, modelled care pathways, and cost calculations). It also presents a sensitivity analysis related to cost calculations and an effectiveness chain analysis related to the assessment of economic effectiveness.
Alén, M. 2022. The economic effectiveness of a care coordination platform in the care process of surgical patients. Master’s thesis, LUT University. Available in Finnish at: https://lutpub.lut.fi/bitstream/handle/10024/164932/Diplomityo_Alen_Mari.pdf?sequence=1
References
1) Korte, H., Jokela, R., Korhonen, E., Perttunen, J. 2020. Lean sosiaali- ja terveydenhuollossa. 2nd edition. HUS Helsinki University Central Hospital.
2) Lauslahti, S. 2007. Kunnan erikoissairaanhoidon kustannushallinnan keinot ja niiden käyttämisen esteet. Doctoral dissertation, University of Tampere.
3) Lillrank, P., Tenhunen, H., Hörhammer, I., Halminen, O., Lyly, T., Linna, M., Silander, K., Laurila, R., Hiltunen, A., Riikonen, E., Miettinen, S., Tanila, T., Chen, A., Vesinurm, M. 2019. Terveydenhuollon digitaalisten ratkaisujen vaikuttavuuden osoittaminen. Final report of the DiRVa project. HEMA Institute & Aalto University.
4) Booth, N., Aronen, P., Mäkelä, M. 2017. Selvitys kustannusvaikuttavuuden käyttämisestä yhtenä terveydenhuollon palveluvalikoiman määrittelykriteerinä. Reports and Memorandums of the Ministry of Social Affairs and Health 2017:30.